Abstract
INTRODUCTION: This population pharmacokinetics (PopPK) analysis assessed the disposition of InO, a CD22 directed antibody conjugated with calicheamicin, as single agent in pediatric subjects with relapsed/refractory (R/R) B-cell precursor CD22+ acute lymphoblastic leukemia (BCP-ALL). Pooled data from the phase IA and II of the trial ITCC-059 (EudraCT:2016-000227-71) are presented. Clinical results from the Phase IA and Phase II were reported previously (Brivio et al., 2021; Pennesi et al., 2022). The trial was sponsored by Erasmus MC and financed by Pfizer.
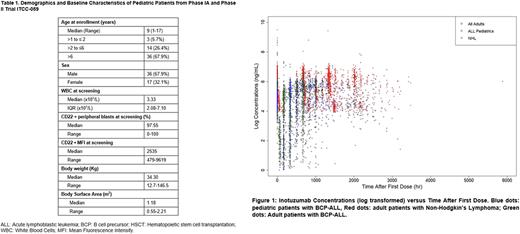
METHODS: Patients aged 1-18 years, in M2 or M3 marrow status, and either ≥ 2nd relapsed, transplanted after 1st relapse, or with refractory disease were enrolled. In Phase I, InO (fractionated in 3 doses/cycle at day 1, 8 and 15) was initially administered at 1.4 mg/m2/cycle (0.6 + 0.4 + 0.4 mg/m2, dose level 1 (DL1)), then escalated to 1.8 mg/m2 (0.8 + 0.5 + 0.5 mg/m2, DL2). In Phase II, patients received 1.8 mg/m2/cycle of InO, or 1.5 mg/m2/cycle (0.5 + 0.5 + 0.5 mg/m2) once remission was achieved. A maximum of 6 cycles were allowed, except for patients proceeding to transplant, for which maximum 2-3 cycles were recommended. A sparse sampling schedule was applied (on day 1, 8, 15 and 22 (cycle 1) or 28 (cycles 2-3)). The PopPK of InO was developed using nonlinear mixed-effects analysis and combining pediatric data from the trial ITCC-059 with data from 11 trials in 765 adult patients with R/R ALL (n=234) or non-Hodgkin's lymphoma (NHL) (n=531) provided by Pfizer. A prior PopPK model developed for adults (Garrett et al., 2019) was used as a basis for pediatric data. This model had two-compartments with both a linear clearance (CL1) and time-dependent clearance (CLt) that includes a decay coefficient (kdes). Covariates included in that analysis, based on Garret et al., were baseline body surface area (BSA) on CL1, CLt, and volume of distribution in the central compartment; diagnosis (ALL/NHL) and/or bioanalytical assay method on CL1, and the decay coefficient associated with time-dependent clearance (kdes); absence of concomitant rituximab (RITXI) on CL1; and baseline percentage of blasts in the peripheral blood (BLSTPB) as a covariate on kdes of CLt. Simulations were performed to predict InO exposures in both pediatric and adult patients at a fixed dosing regimen of 1.8 mg/m2/cycle.
RESULTS: Pharmacokinetic pediatric data were collected from 53 patients (See table 1 for baseline characteristics); 13 treated at DL1, and 40 at DL2; in total 563 serum PK observations were collected. When combined with adult data, the final analysis included a total of 818 patients and 8924 serum PK observations, of which 3394 (38.0%) below the lower limit of quantitation (LLOQ); and hence the M3 method (maximizing the likelihood for data ≥ LLOQ and treating PK data < LLOQ as censored) was selected. Overall, the previous model developed for adults described the pediatric patients’ PK well. Besides the covariates identified in the adult model (BSA, RTX, diagnosis and BLSTPB), the current model also identified the effect of pediatric patients on kdes as a significant covariate. In the final model, InO typical value of CL1 was estimated to be 0.113 L/hr with 40% inter-individual variability (IIV); CL2 was estimated to be 0.384 L/hr with 74% IIV; and central volume of distribution (V1) was estimated to be 6.56 L with 41% IIV. The kdes was estimated to be 0.036 h-1 with 54% IIV. The inter-compartmental CL and peripheral volume of distribution were estimated to be 0.045 L/hr and 4.70 L, respectively. The simulated median Cmax and the accumulated area under the curve (AUC) at end of cycle 1 were 191 ng/mL and 24550 ng.hr/mL; 155 ng/mL and 18200 ng.hr/mL for pediatric and adult patients with ALL, respectively. The simulated median Cmax and accumulated AUC at end of cycle 2 were 284 ng/mL and 117830 ng.hr/mL; 217 ng/mL and 90270 ng.hr/mL for children and adults, respectively.
CONCLUSIONS: InO PK is generally comparable between pediatric and adult patients with R/R ALL. This supports the same dosing regimen in these two populations at 1.8 mg/m2/cycle until remission then 1.5 mg/m2/cycle, the same as per our phase I and II trials.
Disclosures
Pelletier:Pfizer Inc: Current Employment. Chen:Pfizer Inc: Current Employment. Sleight:Pfizer Inc: Current Employment. Locatelli:Neovii: Speakers Bureau; Medac: Speakers Bureau; SOBI: Speakers Bureau; Miltenyi: Speakers Bureau; Jazz Pharmaceuticals: Honoraria; Novartis: Honoraria, Speakers Bureau; BlueBird bio: Speakers Bureau; Amgen: Speakers Bureau. Rossig:novartis: Other: consulting fees; Roche: Other: Consulting Fees; Amgen: Other: Consulting Fees; Pfizer Inc: Other: consulting fee. Sramkova:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Rives:Amgen: Other: Advisory Board; Novartis: Other: Advisory Board. Rizzari:Agmen: Honoraria; Jazz: Honoraria; Servier: Honoraria. Bautista Sirvent:Roche: Other: Consulting Fees; Amgen: Other: Consulting Fees; Bayer: Other: Consulting Fees. Garrett:Pfizer Inc: Current Employment. Zwaan:Pfizer Inc: Honoraria; Novartis: Honoraria; Abbvie: Honoraria; Abbvie: Honoraria; JAZZ: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.